Osteochondrosis is a disease of the spine, in which degenerative processes occur in the cartilage and joints. It is characterized by thinning of the intervertebral discs and a decrease in their elasticity.
Features of the disease
This disease affects mainly the elderly. Although scientists note that the manifestations of the disease more and more often begin from the age of thirty, or even earlier. This suggests that the disease has become much younger.

The intervertebral discs provide a shock-absorbing function, but in case of illness, they are not able to cope with their task. A person suffering from osteochondrosis almost always complains of pain, while pain can manifest itself locally and remotely. A person feels stiffness in movements, lethargy and fatigue.
Basically, pain manifests itself in the section that is affected by the disease.
Localization of pathology and its types
Depending on which part of the spine is damaged by pathology, 4 types of osteochondrosis are distinguished:
- Cervical osteochondrosis. . . Occurs in the case of pathological changes in the cervical spine. The vertebrae become fragile, the load on the cervical spine increases, which can lead to disruption of the thyroid gland, pinching of the artery that supplies blood to the brain.
- Chest osteochondrosis. . . Pathological changes occur in the thoracic spine. It is diagnosed in patients less often than other types, since the thoracic vertebrae are less mobile and protected by stronger muscles. Symptoms of this type are similar to cardiovascular disease.
- Lumbar osteochondrosis. . . This type is the most common. Since the lumbar spine has the greatest load.
- Combined. . . It occurs in the case of damage to several parts of the spine at once.
Along with this, the disease can affect other joints. Most often they suffer:
- Shoulder joint. . . As a rule, the disease is caused by the transition of osteochondrosis of the cervical spine to the shoulder joint.
- Hip joint. . . It occurs due to changes in cartilage tissue and a lack of fluid between the joints.
- Knee-joint. . . Chondrosis can manifest itself in 3 forms:
- Koenig's disease, in which cartilage tissue is affected.
- Larsen-Johansson disease, in which changes occur in the joint above the knee.
- Osgood-Schlatter disease, related to changes in the tibia.
Classification and degree of manifestation of the disease
The disease can be classified according to the degree of its manifestation. At the same time, determining the degree of the disease before the onset of characteristic pain is difficult. There are 4 degrees of manifestation of the disease:
- The initial stage of the development of the disease. It occurs due to the displacement of the spinal disc associated with careless lifting of weight. It is characterized by unstable pain sensations. At this stage, the disease is difficult to diagnose, but it is easily treatable.
- This stage is characterized by the gradual destruction of the intervertebral disc, drying out and loss of shock-absorbing properties. This leads to an increase in tension on blood vessels and nerve endings. Pain sensations intensify and are most pronounced with physical exertion and sudden movements. Treatment of the disease at this stage is conservative.
- The annulus fibrosus is destroyed, and an intervertebral hernia appears. There is a deformation of the spinal column. The pains become significant. Treatment is possible only with the help of surgery.
- At this stage, the vertebrae grow together due to the formation of osteophytes. There is a pinching of the tissues of the spine, the vertebrae lose their mobility and restrict the movement of a person. At this stage, the disease can cause disability and is no longer amenable to treatment.
Typical symptoms
Each type of disease has its own symptoms. So, for example, cervical osteochondrosis is characterized by:
- Painful sensations in the arms and shoulder girdle.
- Headache.
- Dizziness and spots before the eyes.
- Instability of blood pressure.
- Loss of sensitivity in the fingers.
- Tinnitus.
For the pathology of the thoracic region, symptoms are characteristic:
- Pain in the region of the heart.
- Painful feelings in the hypochondrium.
- Lack of air due to sharp pains, shooting in nature.
When the disease is localized in the lumbar spine, there are:
- Painful feelings in the lower back.
- Decreased sensitivity in the legs.
- Radiating pain in the legs.
- Violation of the pelvic organs.
There are also general symptoms that do not depend on the localization of the disease:
- Back soreness.
- Muscle spasms.
- Restriction of movement.
- Change in pain syndrome depending on the load and sudden movements.
- Numbness of the limbs.
- Rapid fatigue.
- Decreased sensitivity of the limbs.

Signs and manifestations of osteochondrosis
The first signs of the disease begin to appear at the first stage of development. These include:
- Swelling and pain in the lower back after lying in one position for more than half an hour.
- The presence of pain in the back after a long sitting.
- The need to stretch after waking up and the inability to immediately wake up and get up.
- Perceived crunch in the back.
- Goosebumps and diminished sensation of the limbs.
- Unpleasant sensations in the back when bending over.
- General weakness.
- Violation of reproductive function and the work of internal organs.
Also, osteochondrosis can be manifested by arising pains when lifting weights and physical activity.
Methods for diagnosing pathology
A complex of methods is used to diagnose osteochondrosis. It includes:
Initial examination and questioning of the patient:
- Interviewing the patient to clarify complaints, the duration of the onset of symptoms.
- Examination of the patient's body, study of posture, gait and movement.
- Palpation of problem areas.
- Determination of pain sensitivity.

Instrumental diagnostics:
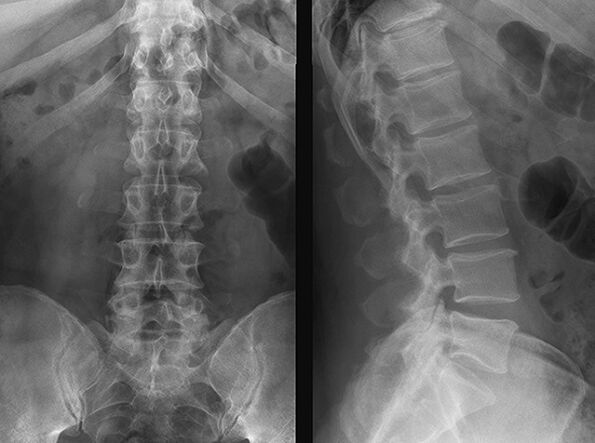
- X-ray to help identify deformation of the intervertebral discs.
- MRI to determine the presence of a herniated disc and its location.
- Computed tomography is similar in its performance to magnetic resonance imaging, but has a greater degree of radiation.
Methods for treating the disease
After carrying out diagnostic procedures and diagnosing osteochondrosis, the doctor prescribes proper treatment.
Since osteochondrosis is treatable only in the first stages of development, all the main measures are aimed mainly at relieving pain. To do this, apply:
- Medication.
- Physiotherapy.
- Manual therapy.
- Massotherapy.
- Diet.
As a drug treatment, non-steroidal anti-inflammatory drugs are used. They are aimed at relieving the inflammatory process in the area of the disease and blocking pain.
Chondroprotectors are also used to restore cartilage tissue. To maintain the normal functioning of the body, immunostimulants and vitamin complexes are used.
Physiotherapy methods are aimed at suppressing pain, normalizing metabolic processes in the affected areas, improving blood circulation, relieving inflammation and edema. These include:
- Acupuncture.
- Magnetic therapy.
- Electrophoresis.
- Laser therapy.
- Paraffin therapy.
Physiotherapy methods help shorten treatment times and have fewer side effects than drug treatments.
Manual therapy is a dosed effect of the doctor's hands on the affected areas of the back, in order to remove restrictions that interfere with the normal functioning of joints, muscles, ligaments.
Therapeutic massage should be carried out only by a specialist, and is aimed at relieving muscle tension, restoring displaced vertebrae and normalizing blood circulation. The procedure should be performed at least three times a week.
The diet for osteochondrosis is aimed at normalizing weight, improving blood circulation, replenishing collagen, eliminating calcium and mineral deficiencies, and helping to control fluid and salt intake. The diet should be balanced and contain plenty of plant foods. In the fight against osteochondrosis, it is necessary to exclude such foods as: coffee and strong tea, foods rich in salt and sugar, carbonated drinks and fatty foods.
The disease, during these procedures, can be corrected and only in difficult stages requires surgical intervention.
Preventive measures
To prevent this ailment, it is necessary to lead a healthy lifestyle and give up bad habits, apply physical activity, use an orthopedic mattress and a pillow for sleeping, avoid using uncomfortable shoes, it is better to use orthopedic shoes.
You should also monitor your diet and maintain a healthy weight. With a long stay in a static state, it is necessary to allocate time for exercises that help normalize blood circulation.
Also, for the prevention and prevention of the disease, you can undergo sanatorium treatment and general strengthening massage.
























